Abstract
Introduction
Beta thalassemia is an inherited disorder characterised by ineffective erythropoiesis leading to anemia and secondary iron overload. Neutrophils are the first line of innate immune defence against infection is dysfunctional in thalassemia patients. Iron is required for the oxidative response of neutrophils to allow the production of reactive oxygen species (ROS). However, the role of iron contributing to the neutrophil dysfunction is unclear. This is the first study to characterise the neutrophil iron metabolism in β-thalassemia and its association with oxidative burst capacity, phagocytosis, and systemic iron homeostasis.
Method
Sixteen thalassemia patients and fourteen healthy individuals were recruited in the department of Haematology, Christian Medical College, Vellore, India. Neutrophils were purified from human whole blood collected in EDTA tube, using neutrophil magnetic isolation kit (Miltenyi Biotec). Purified population (>95%) was confirmed by the presence of the surface marker CD62L evaluated using flow cytometry. Haematological parameters were analysed according to standard methods. Serum ferritin, iron, soluble transferrin receptor were measured using immunoassay. Serum hepcidin was measured using ELISA. Neutrophil RNA was isolated using trizol method and was reverse transcribed into complementary DNA using QIAGEN kit. The relative quantification of iron related genes were measured using real-time PCR. In oxidative burst assay, neutrophils were incubated with dihydrorhodamine 123 (DHR) and stimulated with Phorbol 12-Myristate 13-Acetate (PMA). Respiratory burst of the cell was analysed by flow cytometry. Phagocytosis and acidification capacity of human neutrophils were quantified using the pHrodo Green Staphylococcus aureus BioParticles kit (Thermo Fisher). Acquisition was performed using the Beckman Coulter(Navios) flow cytometer and analysed using kaluza software. Statistical analysis was performed using SPSS software.
Results
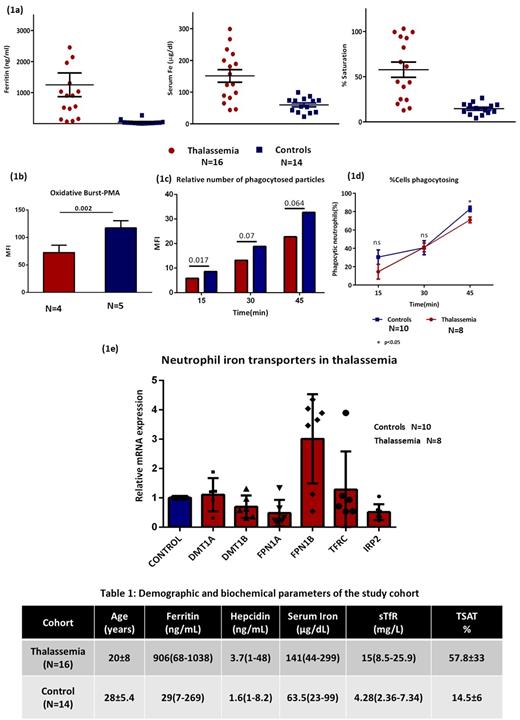
We investigated a cohort of β thalassemia Major (n=5), intermedia (n=6) and sickle beta thalassemia (n=5) patients who were on regular iron chelation therapy. The demographic and biochemical parameters are tabulated in Table 1. Serum iron, ferritin levels and transferrin saturation were significantly increased in thalassemia cohort as compared to healthy donors (Fig1a). There was no significant association between ferritin and hepcidin levels. The percentage of neutrophils in thalassemia was significantly reduced incomparision to healthy donors (p=0.032). Oxidative burst capacity of neutrophils from thalassemia major and intermedia patients were significantly decreased (p=0.002) compared to healthy donors upon stimulation with PMA (Fig1b). Neutrophil phagocytosis capacity indicated by the relative amounts of phagocytized fluorescein S.aureus particles were significantly lower in thalassemia patients compared with controls, after 15min/30min incubation (Fig1c). The recognition capacity of neutrophils towards bioparticles significantly decreased at 45-minute incubation in patients (p=0.017) (Fig1d). Serum iron overload and transferrin saturation had negative association with neutrophil phagocytosis capacity (r=-0.714; p=0.045 & r=-0.857; p=0.014), respectively. Neutrophil iron related gene expression was analysed and found significantly lower expression of FPN 1A (FPN1 containing iron regulatory element (IRE)), DMT1B without IRE region and IRP2 respectively (p=0.029, p=0.029 & p=0.016) (Fig1e). FPN1B without IRE region was upregulated in thalassemia patients (p=0.016). Serum ferritin had positive correlation with FPN1B (r=0.786; p=0.036). Soluble transferrin receptor had negative association with DMT1A (containing IRE region) and IRP2 respectively (r=-0.900; p=0.037 and r=-0.750; p=0.052).
Aberrant neutrophil function was found in all thalassemia patients. Although oxidative burst activity was decreased in thalassemia major and intermedia patients, sickle β-thalassemia patients had normal burst activity. Systemic iron status had inverse correlation with phagocytosis capacity of neutrophils. Dysregulation of iron transporters in neutrophils was indicated by decreased expression of DMT1 and augmented FPN1B expression, despite systemic iron overload. These findings have to be explored in a larger cohort to elucidate the clinical significance.
No relevant conflicts of interest to declare.